Page Content
Research Team
- Peter Wayne, PhD, Center Director
- Yan Ma, MD, T-32 Post-Doctoral Research Fellow
- Dennis Muñoz Vergara, DVM, PhD, T-32 Post-Doctoral Research Fellow
- Daniel Litrownik, BA, Project Manager and Lab Coordinator
- EunMee (Amy) Yang, T-32 Post-Doctoral Research Fellow
- Natalie Mitchell, MS, Research Assistant
About the Team
Peter Wayne, Principal Investigator
Daniel Litrownik, Project Manager and Lab Coordinator, received his B.A. in Psychology from Emory University. He brings 10+ years’ experience in coordinating clinical trials of mind-body interventions with different patient populations. He is most interested in the development and refinement of mind-body interventions for specific patient populations, and the optimization of recruitment and retention strategies for pilot feasibility studies and larger efficacy trials. He is a long-term practitioner of meditation and Tai Chi and finds meaning in bridging his personal and professional interests.
EunMee (Amy) Yang, T-32 Post-Doctoral Research Fellow, is a licensed acupuncturist and diplomate of Oriental Medicine. Her research interests are primarily focused on evaluating the effectiveness of acupuncture for improving cancer-related symptoms and exploring the biological basis and biophysical properties of acupuncture points.
Dennis Muñoz Vergara, a T-32 Post-Doctoral Research Fellow, is a Doctor of Veterinary Medicine and an animal pathologist and a certified Hatha yoga instructor. He is interested in translational research using in vitro, ex vivo and in vivo animal and human models to understand the basic biological mechanism of stretching and its effects on inflammation. His current human research study attempts to isolate the stretching component of yoga and apply an acute intervention (one hour of stretching) to explore changes in systemic inflammatory markers and lipid mediators.
Yan Ma, T-32 Post-Doctoral Research Fellow, received her MD in integrative medicine, and specialized in sleep medicine and clinical psychology. She is interested in mind-body interventions and techniques which are capable of capturing system-level complex physiological dynamics.
Natalie Mitchell, Research Assistant, received her M.S. in counseling psychology from Northeastern University. Her research interests include the impact on mindfulness on wellness and the formation of identity. She has prior experience in qualitative research methods as well as clinical psychology experience that aid her in her interactions with research participants.
Research Overview
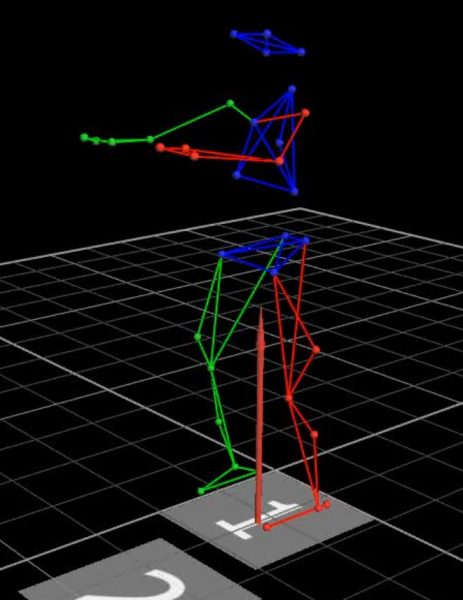
The Mind-Body-Movement (MBM) laboratory explores the interdependence of movement, posture, cognition and emotion in health, aging and rehabilitation. Our research begins with the assumption that health relies on the complex integration of these and other physiological systems, enabling us to function and adapt to the demands of everyday life. Conversely, age-related decline and disease is thought to result from progressive multi-system impairment, leading to decreased physical and cognitive function and reduced resilience to stress.
Taking advantage of a rich collaborative network of laboratories across the Harvard Medical School, and drawing on conceptual models, quantitative methods, and experimental designs grounded in systems biology, our research has focused on evaluating the clinical impact and physiological basis of multiple integrative medicine (IM) therapies.
Current work centers around the study of Tai Chi and related mind-body exercises, manual therapies, and acupuncture for the prevention, rehabilitation, and symptom management of a broad range of chronic health conditions including age- and Parkinson’s disease-related balance impairments, cognitive decline, chronic back and neck pain, cardiovascular diseases, migraine headaches, and cancer.
Research on these, ongoing research studies, and related topics are summarized below.















